When states seek federal funding for health workforce initiatives such as for the Rural Health Transformation Program funding opportunity, federal workforce shortage designation data (such as Health Professional Shortage Areas, HPSAs, or Medically Underserved Areas/Populations, MUA/Ps) has become the go-to state metric for demonstrating need. And for good reason; these federal designations offer a standardized, comparable measure that can be used across all 50 states to identify where healthcare workers are most critically needed. These designations provide valuable details about provider categories and geographic areas, enabling targeted investments that address specific gaps in the healthcare workforce.
However, there’s a critical factor that often goes unexamined: the quality and comprehensiveness of the data foundation underlying these designations. Like any analysis tool, these figures are only as reliable as the data that feeds them. As research published in Health Affairs Forefront has underscored, persistent gaps and inconsistencies in workforce data collection across states limit our collective ability to accurately “count our doctors,” and, more importantly, to fix workforce shortages (Why We Can’t Count Our Doctors—and How to Fix It).
Across the United States, states take dramatically different approaches to collecting workforce data, with significant implications for their ability to understand, plan for, and address their healthcare workforce challenges.
The Data Collection Divide
State approaches to health workforce data collection exist on a spectrum. At one end, some states maintain only the bare minimum required to satisfy federal health workforce shortage designation requirements. These states may collect limited information from select provider types, focusing solely on what’s needed to calculate ratios and identify shortage areas. Their data collection approaches and data systems are purpose-built for HPSA/MUA/P designations; nothing more, nothing less.
At the other end of the spectrum are states that have built comprehensive workforce data systems. These states collect information from numerous licensed healthcare professionals during the licensing process, creating a rich, complete picture of their healthcare workforce. Rather than treating data collection as a compliance exercise, these states view it as a strategic asset for workforce planning and policy development.
The differences between these approaches are not merely academic. A state with minimal data collection may successfully calculate designations but lack the detailed information needed to understand why shortages exist, which specific specialties are affected, or how workforce patterns are changing over time. In contrast, a state with comprehensive data collection can not only identify shortages but also proactively anticipate shortages, determine service or specialty shortages, and develop targeted solutions.
Bare Minimum Health Workforce Data Collection: License counts + HPSA/MUA/P Data
Comprehensive Data for State Planning: Can calculate HPSA/MUA/Ps + predict retirements + identify specialty gaps + track diversity + measure policy impact + guide training programs + more
From Single-Purpose to Multi-Purpose Data Systems
The value of workforce data extends far beyond HPSA and MUA/P calculations. States with robust data systems use this information for multiple purposes, sharing data across agencies and government branches to inform various policy and planning decisions. These multi-purpose systems can answer critical questions that single-purpose data collection cannot:
- What is the age distribution of primary care physicians in rural counties, and when might retirements create additional shortages?
- How much of our workforce trained in-state, and to what extent are we “growing our own” vs. relying on imports?
- How many mental health counselors are practicing in underserved areas?
- Where are newly licensed healthcare professionals choosing to practice?
- How do workforce patterns vary across different healthcare professions that may not be included in HPSA calculations?
States with comprehensive systems can answer these questions because their data infrastructure supports multiple uses. The same information collected during licensing can support federal shortage designations, inform grant applications, guide education and training programs, support rural health initiatives, answer legislative inquiries, and help plan for future workforce needs. This multi-purpose approach maximizes the value of data collection efforts and ensures that workforce planning is based on complete, accurate information.
The Licensing Process: A Strategic Opportunity
The most effective approach to building a comprehensive workforce data foundation is to integrate data collection into the professional licensing process through tools designed to address HPSA data needs and beyond, such as the Cross-Profession Minimum Data Set. This data collection approach offers several distinct advantages that make it the best practice for states seeking to understand and plan for their healthcare workforce needs.
Licensing-based data collection offers several distinct advantages:
Near-universal coverage. Because licensure is required to practice, collecting data during the licensing process captures information from nearly all providers, eliminating sampling bias and data gaps.
It is important to acknowledge, however, that licensure compacts introduce additional complexity into state-based data collection, as some clinicians may practice under compact privilege rather than a traditional state-issued license. Encouragingly, many compacts are strengthening their own data collection and data-sharing capabilities, creating opportunities for compact-level data to complement state licensing data and support a more complete picture of the active workforce.
Regular updates. License renewals, typically every one to three years, create a built-in refresh cycle that allows states to track changes in practice location, service delivery, and workforce composition over time.
Administrative efficiency. Embedding data collection into an existing process minimizes burden on both providers and state agencies, yielding high response rates without the need for stand-alone surveys.
Long-term sustainability. Unlike grant-funded or one-time studies, licensing-based collection establishes a long-term data infrastructure that supports trend analysis, program evaluation, and continuous improvement.
Healthcare professionals renew their licenses every 1-3 years. Each renewal is a new opportunity for the state to refresh and update their data for planning, at a low administrative burden to both the state and the professionals.
Routine license renewals = automatic data updates. Low burden for providers, high value for state planning.
Building Better: The Path Forward
For states currently operating with minimal workforce data systems, the path to improvement is clear: invest in building a comprehensive data foundation through the licensing process. This requires collaboration between licensing boards, health, human services, and workforce agencies, and other stakeholders, but the investment pays dividends across multiple policy areas.
States should design their licensing-based data collection systems with multiple purposes in mind from the start. While data for federal health workforce shortage designations should be front and center and is often the drive for these investments, states should consider how this investment could be leveraged to support broader workforce planning, education program assessment, rural health initiatives, and other state priorities.
Conclusion: Data as Strategic Infrastructure
Federal workforce shortage designations will continue to play a vital role in targeting resources and demonstrating need for workforce investments. Their standardization and comparability make them indispensable tools for states.
But the reliability and usefulness of HPSA/MUA/P data depend entirely on the strength of the underlying workforce data infrastructure. States that treat workforce data as strategic infrastructure (grounded in licensing-based collection, aligned with national standards, and adaptable to emerging models like compacts) are better positioned to understand their challenges, implement targeted solutions, and measure impact over time.
In an era of growing healthcare workforce challenges, comprehensive, high-quality data is not a luxury, it’s essential infrastructure for effective planning and policy-making. States that recognize this and invest accordingly will be better equipped to ensure that their residents have access to the healthcare services they need, now and in the future.
Indiana Spotlight: Building Workforce Data That Works
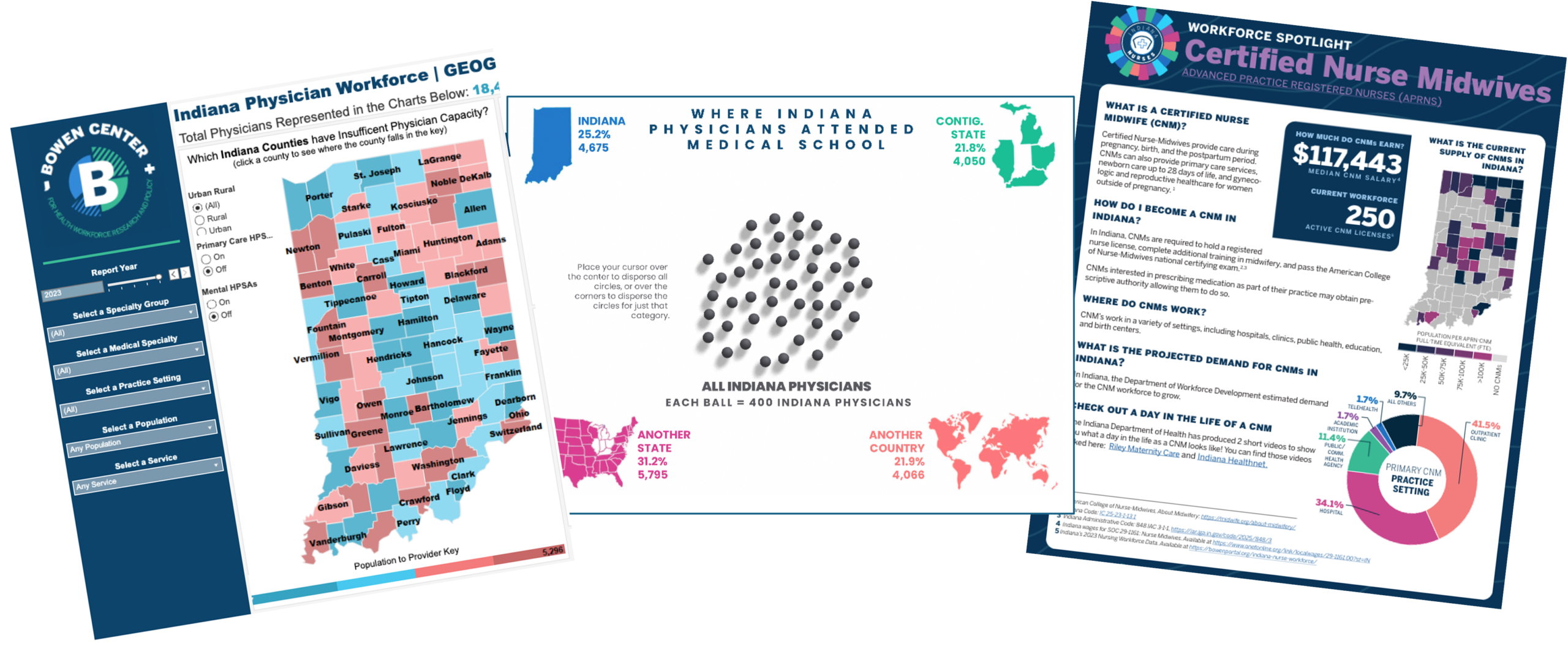
Indiana stands out as a national example of how states can turn licensure data into actionable insight. Through a partnership between the Indiana Professional Licensing Agency and the IU Bowen Center for Health Workforce Research & Policy, Indiana collects comprehensive workforce data during the licensing process that is cleaned and shared back to the state Primary Care Office for HPSA analysis and other agencies for workforce planning. The Bowen Center translates this data into trusted analysis and reports that inform policy, education planning, and access-to-care decisions statewide. It’s a model of how investing in health workforce data infrastructure pays dividends far beyond compliance.
Indiana’s experience shows what’s possible when states treat health workforce data as strategic infrastructure to drive smarter investments and enhance access to care. If you’re interested in exploring opportunities to strengthen or enhance your state’s health workforce data, our inbox is always open.

